Subdural Hematomas - Bilateral
Title: Middle Meningeal Artery Embolization of Subdural Hematomas
Case Presentation:
A woman in her 80s developed mild dizziness and headache following incidental trauma working in his garage one day. She presented several weeks later to the ER and was diagnosed with bilateral subdural hematomas, which were initially managed with observation, low dose Decadron, considering the mildness of symptoms, advanced age, and history of CLL with thrombocyptopenia (<100k). Over the next 4 weeks, the collections remained relatively stable with evidence of slight growth (10 to 12 mm thickness, and 2 mm right to left shift) on NCT (Figure 1. A and B).

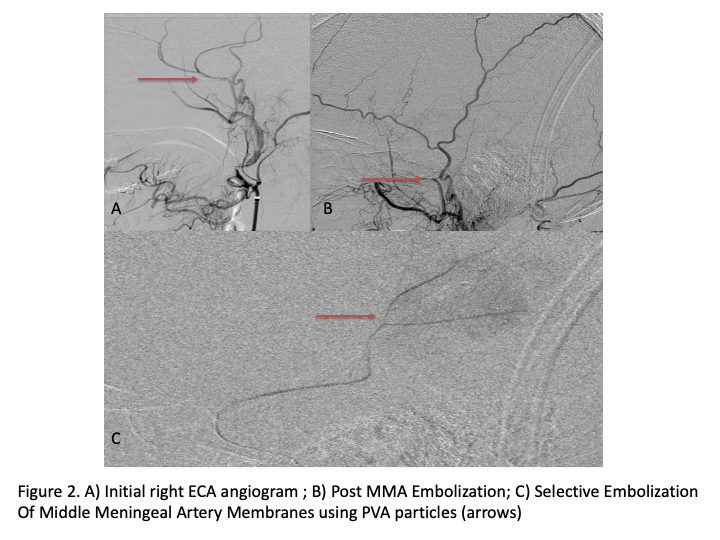
The patient agreed to receive minimally invasive treatment with Bilateral Middle Meningeal Artery Embolization, a new approach to promote resorption of chronic and subacute subdural hematomas in patients that are not improving with conservative measures or have contra-indications to surgical evacuation. Selective catheterization of the Middle Meningeal Artery is followed by transarterial embolization of the territory and inflammatory membranes that are felt to be secreting serosanguinous proteinaceous exceeding the capacity for resorption. MMA embolization was performed bilaterally in this patient. (Figure 2. A and B)
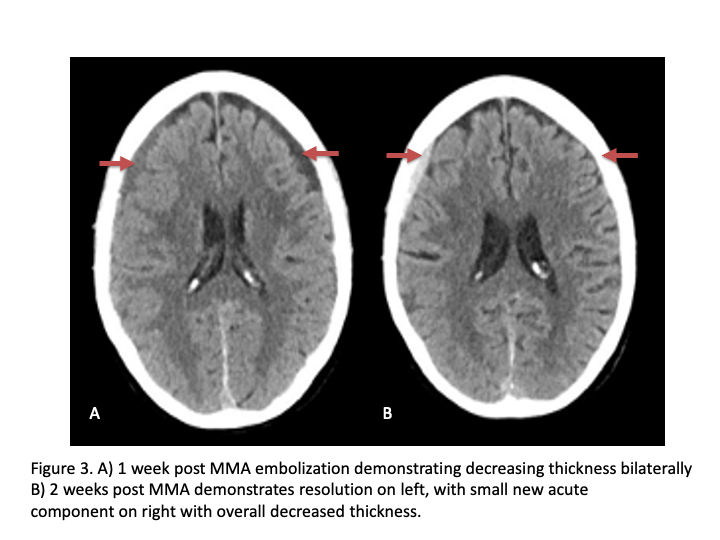
CT follow-up at 1 week demonstrates early resorption. 2 weeks post MMA embolization, resolution of the left subdural collection with new small thin acute hemorrhage in an otherwise stable right subdural collection is observed (Figure 3. A and B).
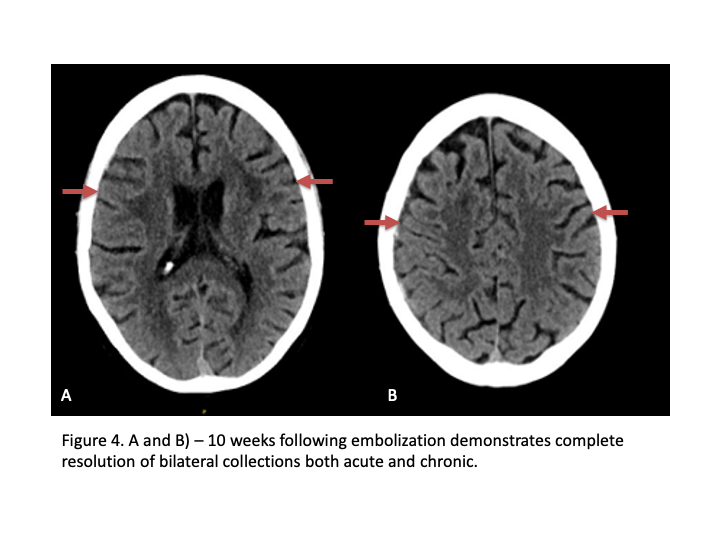
Clinically, the patient improved over the few weeks with the occasional transient twinge of a headache, but resolution of dizziness. Follow-up CT at 10 weeks demonstrated complete resolution of the bilateral subdural hematomas with our patient complete symptomatic and back to all of his activities of daily living. Considering his history of thrombocytopenia and CLL, we will continue to monitor him into the future and are excited about his progress and recovery. (Figure 4. A and B) Long-term followup at 6 months confirmed complete healing and resolution of all symptoms without the need for invasive brain surgery.