Carotid Cavernous Fistula - AVM
Title: Direct Carotid Cavernous Fistula (CCF)
Clinical Case Study:
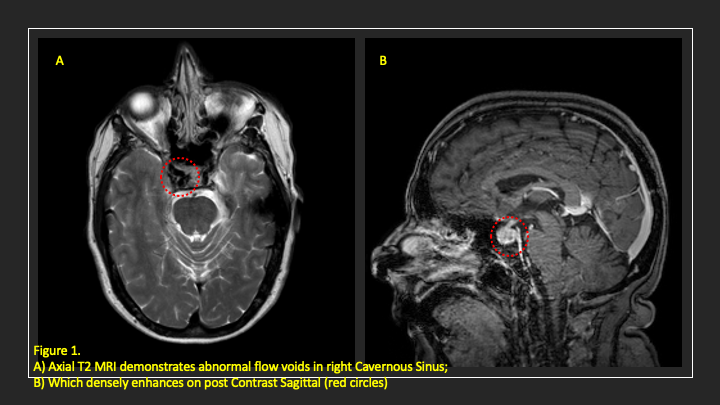
A 60-year-old woman who is otherwise healthy who presented with progressive right-sided pulsatile tinnitus for 4-6 weeks. She underwent extensive evaluation by her PCP and ENT which included multiple courses of steroids and subsequent advanced MRI and MRA imaging. Several days prior to presentation, she developed new onset diplopia which was found to be secondary to a partial right VI nerve palsy. MRI demonstrates abnormal flow voids in the right Cavernous Sinus, which also enhances densely (Figure 1).
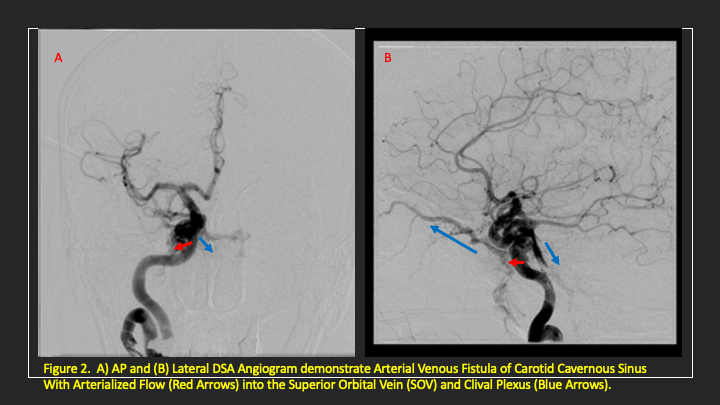
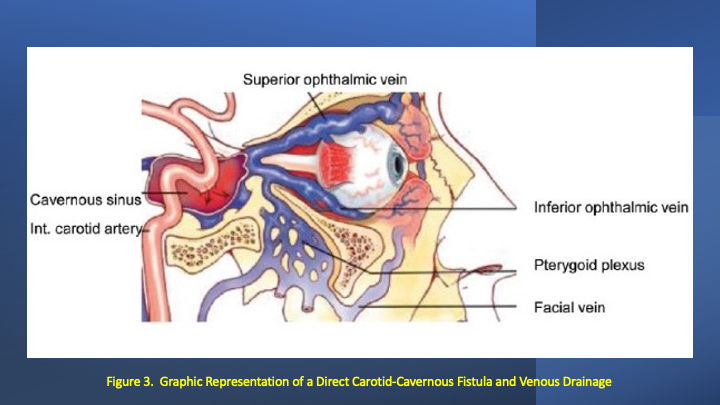
We performed a diagnostic cerebral angiogram which confirm the presence of a high flow direct fistula of the right internal carotid artery–right cavernous sinus. Collateral venous drainage into the orbit and skull base was observed (Figures 2 and 3).
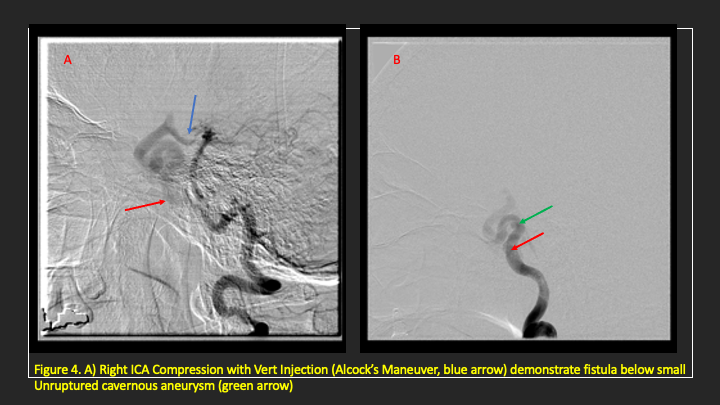
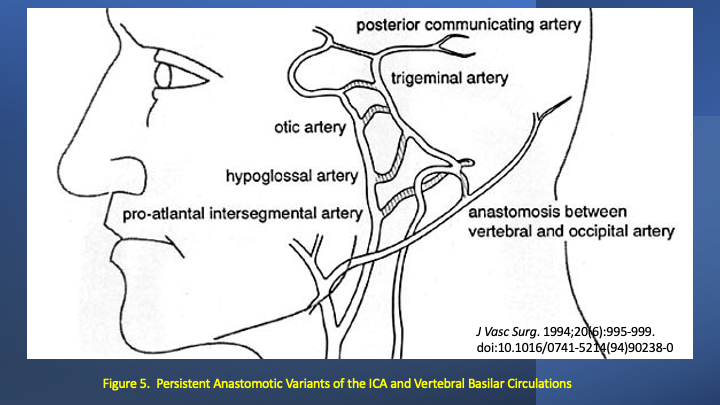
We decided to proceed with an endovascular approach which required identifying the direct site of the fistula. Secondary to the high flow nature of the fistula, and the presence of a small intra-cavernous aneurysm, we performed an Alcock’s maneuver where the vertebral artery was injected during compression of the Right Carotid Artery to reverse flow and identify the fistula site. In this patient, the incidental superior cavernous aneurysm was unruptured, and the site of the fistula was identified more proximally in the location of a potentially ruptured Otic Artery aneurysm. (Figures 4 and 5).
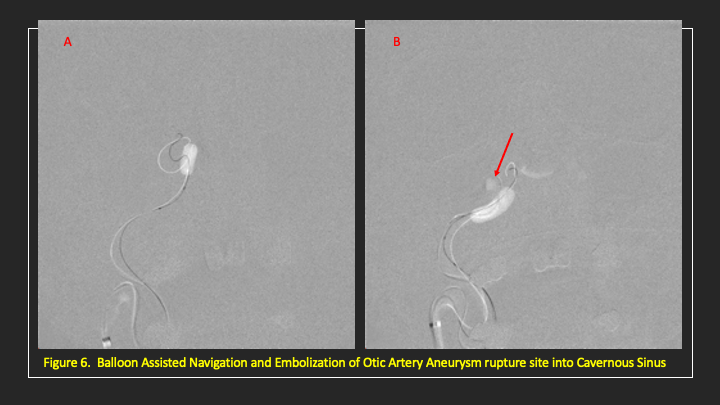
We then proceeded to successfully cannulate the direct aperture between the right carotid artery and the cavernous sinus and with the use of a balloon assist technique coil embolized the posterolateral compartment until the fistula was closed and shunting ceased (Figures 6 and 7).
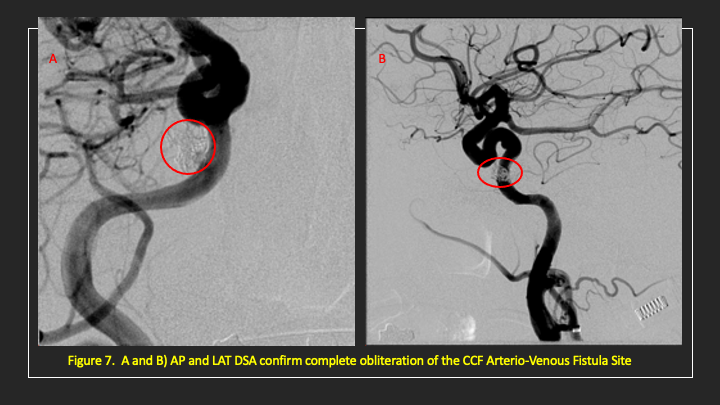
She experienced immediate cessation of her pulsatile tinnitus with early improvement of the right VI nerve palsy and near complete recovery within 4-6 weeks (diplopia only on far lateral gaze) and permanent cure at 6 months.
Discussion:
Carotid-cavernous sinus fistulae (CCF) occur because of traumatic or spontaneous communication in the walls of the intra-cavernous internal carotid artery or its branches directly to the cavernous sinus resulting in short-circuiting or shunting of high-pressure arterial blood into the venous system of the cavernous sinuses. Intra-cavernous cerebral aneurysms are often felt to predispose to a Direct Carotid-Cavernous Sinus Fistulae, which represent the majority of fistulae in most series. These fistulae usually have high rates of arterial blood flow and most commonly are caused by a single tear or aperture in the arterial wall and can result in rapid progression of clinical symptoms including cranial nerve injury and vision loss.[i]
The most used classification, based on angio-architecture, was established by Barrow et al. dividing CCFs into 4 types based on the arterial supply:[ii]
- Type A (direct): Direct communications between the internal carotid artery (ICA) and the cavernous sinus, usually with resulting high flow rates.
- Type B (indirect): only by dural branches of internal carotid artery (ICA).
- Type C (indirect): only by dural branches of external carotid artery (ECA).
- Type D (indirect): by dural branches of both ICA and ECA.
Indirect or Dural carotid-cavernous sinus fistulae are characterized by a communication between one or more meningeal branches of the internal carotid artery and/or the external carotid artery with the cavernous sinus. These fistulae usually have lower rates of arterial blood flow initially but may progress to develop higher pressure and cortical venous reflux and associated risks of visual deficits and hemorrhagic strokes.[iii] These lesions may represent congenital or acquired arteriovenous malformations, which develop spontaneously or in association with atherosclerosis, systemic hypertension, collagen vascular disease, cavernous sinus thrombosis, and peri-partum situations in women.
Early evaluation by a neurovascular specialist is recommended for patients presenting with new onset or progressive pulsatile tinnitus, especially in patients with associated visual symptoms (chemosis, proptosis, diplopia) and can often lead to successful treatment and prevention of serious life-threatening complications of the disease.
Key Learning Points:
- Carotid-Cavernous Sinus Fistula (CCF) may occur because of traumatic or spontaneous communication in the walls of the intra-cavernous ICA or its branches directly to the cavernous sinus resulting in short-circuiting or shunting of high-pressure arterial blood into the venous system of the cavernous sinuses.
- Intra-cavernous aneurysms are often felt to predispose to a Direct CCF which have high rates of arterialized blood flow and can result in rapid progression of clinical symptoms including cranial nerve injury and vision loss.
- Early evaluation by a neurovascular specialist is recommended for patients presenting with new onset or progressive pulsatile tinnitus, especially in patients with associated visual symptoms or new neurologic deficits.
References:
[i] Gemmete, Joseph J MD; Ansari, Sameer A MD, PhD; Gandhi, Dheeraj M MD Endovascular Techniques for Treatment of Carotid-Cavernous Fistula, Journal of Neuro-Ophthalmology: March 2009 – Volume 29 – Issue 1 – p 62-71. doi: 10.1097/WNO.0b013e3181989fc0
[ii] Barrow DL, Spector RH, Braun IF, Landman JA, Tindall SC, Tindall GT. Classification and treatment of spontaneous carotid-cavernous sinus fistulas. J Neurosurg. 1985 Feb;62(2):248-56. doi: 10.3171/jns.1985.62.2.0248. PMID: 3968564.
[iii] Halbach VV, Hieshima GB, Higashida RT, Reicher M. Carotid cavernous fistulae: indications for urgent treatment. AJR Am J Roentgenol. 1987 Sep;149(3):587-93. doi: 10.2214/ajr.149.3.587. PMID: 3497549.
