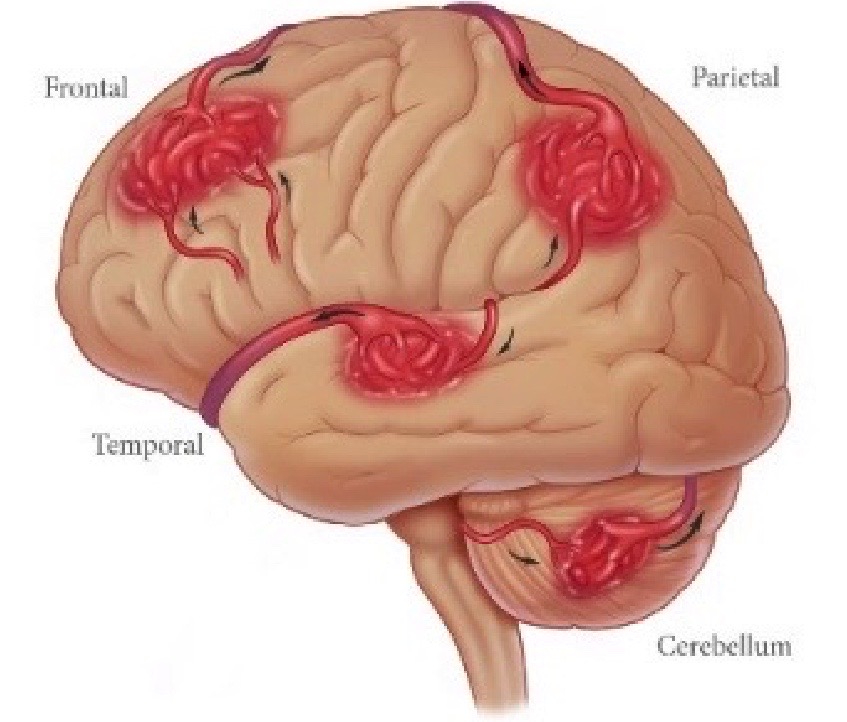
Brain AVM's or Arteriovenous Malformations


What are the Risks of an AVM?
Over time, the high blood flow and shunting of high-pressure arterial blood through the AVM causes the feeder arteries and veins making up the AVM to dilate (or expand). This dilation weakens veins making them susceptible to hemorrhage; feeder arteries become susceptible to aneurysms, a weakened spot in the blood vessel wall that expands and can eventually hemorrhage.There is a 10-15 percent risk of death, and a 20-30 percent chance of permanent brain damage, related to each bleed. Each time blood leaks into the brain, normal brain tissue is damaged. This results in loss of normal function, which may be temporary or permanent. Some possible symptoms include arm or leg weakness/paralysis, or difficulty with speech, vision, or memory. The amount of brain damage depends upon how much blood has leaked from the AVM. Smaller AVMs present with hemorrhage more often than large ones. In addition, the size of the hematoma (a localized swelling filled with blood resulting from a break in a blood vessel) is larger from the small AVM, compared with the medium or large AVM. There appears to be no difference in the frequency of hemorrhage between large and medium AVMs. However, whether size of the AVM is a true risk factor is unclear.
What are the Symptoms of an AVM?
The symptoms of an AVM depends on if it has Hemorrhaged or NOT (Unruptured), and depends on location of the AVM, as well as the severity of the bleed. If an AVM has NOT Bled, it may be discovered incidentally or present with symptoms. These symptoms may include:
- Sudden and severe headache, nausea & vomiting
- Seizure
- Loss of consciousness
- “Stroke-like” symptoms: problems speaking, numbness/tingling, muscle weakness, changes in vision.
Hemorrhage is a result of blood vessels that are weakened by the shunting of high-pressure arterial blood through the abnormal arteries and veins of the AVM. The short-term and long-term neurological effects of the hemorrhage differ depending on how much blood has leaked into the brain and where the hemorrhage is located. Factors for spontaneous bleeding before or in the absence of treatment include:
- History of prior hemorrhage (Highest risk of Re-Bleeding in the first 1-5 years after Initial hemorrhage)
- Deep venous drainage
- Feeding artery aneurysms and intranidal aneurysms
- Venous restrictive disease: blockage in the drainage system
How Can a Brain AVM be Treated?
- Risk Factor Reduction and Close Monitoring with Imaging
- Depending on your Age, Risk Factors, Location, and Size of the AVM, many people may be at Lower Risk for Developing Symptoms or having their AVM Rupture. We may advise that risk factors such as Blood Pressure and Smoking Cessation be managed with Serial Imaging be performed to monitor your Brain AVM. If the AVM shows signs of Growth or has a change in it’s Morphology (shape changes or an irregularity develops) or Bleeds (Hemorrhages), further Treatment options may be considered. Many Brain AVMs that have NOT Bled into the Brain or cause minimal symptoms may be cautiously observed and treated with medications for the symptoms and monitored closely for signs of worsening.
- Neurointerventional or Neuroendovascular Therapy
- If a Person is Young, or has certain Risk Factors such as Congenital Medical Condition (Heriditary Hemorrhagic Telangiectasia -HHT), or Known Bleeding Event, Minimally Invasive Treatment of their AVM may be considered.
- Neurointerventional Therapy is performed by accessing the Blood Vessels through a small incision in the Leg (Femoral Artery) or Arm (Radial or Axillary Artery) and Navigating small “Tubes” or Catheters into the Brain. Several Different Treatment Strategies may be employed to treat a Brain AVMs including Embolization or “Blocking” of their Abnormal Blood Vessels or “Shunts” using Blocking Agents such as “Glue” or NBCA, or Onyx. Sometimes, special adjunctive devices such as a Balloon may also be utilized to effect a more durable result and lower the risks. The Recovery Period for these Techniques is usually very short, as little as 1-2 days in the Hospital. Embolization Therapy may be performed as the Definitive Procedure to Cure some AVM’s or as an Adjunctive Pre-Operative Procedure to make Surgical Excision Safer or Radiosurgery more effective.
- Microsurgical Therapy
- In some Patients, the AVM may not be “Cured” with Embolization Alone and Open-Brain Surgical Therapy or a Craniotomy is performed to Surgically Excise or Remove the AVM.
- Radiosurgery
- In some Patients, especially those presenting with Unruptured AVM’s (those that have NOT Hemorrhaged), and the AVM is Small or greatly reduced in size with Embolization, Doses of Radiation can be Targeted to the Abnormal Blood Vessels to “Scar” them and allow them to Heal. The effects of Radiosurgery, however, are not immediate and may take 3-5 years to ultimately maximize their therapeutic effects.
- Risks of Treatment
- Monitoring
- There is the possibility that an AVM may Rupture or Grow during a surveillance period before there is an opportunity to treat with Neurointerventional or Surgical techniques. This may result in severe Brain Injury or Death associated with the Brain Hemorrhage as described above.
- Neurointerventional Therapy
- When a Person undergoes treatment of their AVM, there are risks that the AVM may rupture or that an important blood vessel may become blocked during the Operation. This could result in Severe Permanent Brain Injury or Stroke, Long-Term Permanent Disability, or even Death. These risks may vary based on the complexity of the Brain AVM.
- Microsurgical or Open Brain Surgery Treatment
- As with Neurointerventional Therapy, the AVM may rupture or an important blood vessel may be occluded during the Operation which can result in Permanent Disability or Death. Open Brain Surgery also carries the additional risks of direct manipulation of the Brain and associated Brain Injury and is generally associated with longer recovery times and side-effects, including a risk of developing seizures.
- Radiosurgery
- Delivering High Doses of Radiation targeted to the AVM may have secondary damage to nearby normal brain tissue resulting in long-term injury or symptoms of “Stroke”. In addition, the delayed Therapeutic Effects of 3-5 years still carries the Risks of the AVM Bleeding during the Healing period.
- Monitoring
Special Thanks to Dina Chon (Executive Director) and The Aneurysm and AVM Foundation (TAAF) for their permission to use their illustrations and educational materials to help spread Awareness for these Life-Threatening conditions. Please visit their Site to learn more and Support this vibrant community.
